Exciting new NZ-Japan research collaboration
RTRU has recently received a new funding grant from the Royal Society Te Apārangi to support a brand new research collaboration between occupational therapy researchers from Japan and Māori, Pacific, and Pākehā researchers in New Zealand. Lead by yours truly (William Levack), this project involves the development and testing of a) an English-language version and b) a Māori/Pacific version of a Japanese iPad application called the “Aid for Decision-Making in Occupational Choice” (ADOC).
ADOC is designed to help health professionals engage with patients (adults and children) and their family/whānau in collaborative goal setting for rehabilitation (e.g. for people with stroke, spinal cord injury, cerebral palsy, or dementia). Despite the importance of goal setting in rehabilitation, past research has demonstrated that involving patients in goal setting can be difficult, with health professionals tending to dominate discussions around the selection of goals, and issues such as communication and cognitive impairments creating obstacles to robust patient involvement. This project will provide the ground work required for future research investigating the use of digital technology as a tool to support rehabilitation professionals to be more culturally responsive and person-centred in their clinical practice – improving the quality of their service delivery and increasing opportunities for more meaningful health outcomes for their patients.
My research collaborators for this project are Bernadette Jones (Ngāti Apa Ngā Wairiki), Dr Tristram Ingram (Ngāti Kahungunu ki Heretaunga, Ngāti Porou), Dr Dianne Sika-Paotonu, A/Prof Rebecca Grainger (from University of Otago), A/Prof Kounosuke Tomori and Dr Tatsunori Sawade (from Tokyo University of Technology), and A/Prof Kayoko Takahashi (from Kitasato University). Funding from the Royal Society Te Apārangi will support travel between New Zealand and Japan to help us successfully complete this work. Additional funding support for our various collaborative projects over the next two years has also be provided by the Japanese Society for the Promotion of Science and by a University of Otago Research Grant.
Self-led management of rheumatoid arthritis
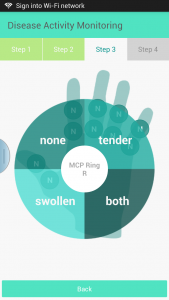
 The management of rheumatoid arthritis (RA) has transformed in recent decades so the inflammatory arthritis is often well controlled with medications used in a treat-to-target strategy. This “T2T” strategy requires measurement of RA disease activity using validated measures and increasing treatment until disease remission or at least a low disease activity state is achieved. Currently the RA activity is determined during clinic visits however these are currently at arbitrary intervals so people are may be seen when they are well and appointments are not always available when people have increased arthritis activity and need medical help. Some data suggest the assessment of RA activity by people with RA correlates fairly well with the assessment of disease activity by health professionals. RTRU academic, Dr Rebecca Grainger, has begun to explore the possibility of the assessment and monitoring of RA being led by the person with the disease rather than the health system. In this new tech world, a phone app seem to be a good option to try. Dr Grainger, in collaboration with her colleagues in RTRU, Hutt Hospital, and the Department of Information Science at University of Otago, first conducted a systematic review of all apps that could enable measurement of RA disease activity by people with RA and for those data to be transmitted to their rheumatology team for monitoring. (This review can be downloaded for free here.) They found the 19 potentially useable app for longitudinal assessment of disease activity,which fell into two categories: 1) simple calculators of disease activity or 2) data tracking tools for people with RA. However, no apps used all the required validated instruments and allowed for data transmission. One high quality app “Arthritis Power” does a great job of longitudinal tracking of validated patient-reported outcomes (PRO’s) and is used for patient-led research but is not suitable for use in “telerheumatology” due to lack of measurement of tender and swollen joints, a key feature of RA activity measured by rheumatologists.
The management of rheumatoid arthritis (RA) has transformed in recent decades so the inflammatory arthritis is often well controlled with medications used in a treat-to-target strategy. This “T2T” strategy requires measurement of RA disease activity using validated measures and increasing treatment until disease remission or at least a low disease activity state is achieved. Currently the RA activity is determined during clinic visits however these are currently at arbitrary intervals so people are may be seen when they are well and appointments are not always available when people have increased arthritis activity and need medical help. Some data suggest the assessment of RA activity by people with RA correlates fairly well with the assessment of disease activity by health professionals. RTRU academic, Dr Rebecca Grainger, has begun to explore the possibility of the assessment and monitoring of RA being led by the person with the disease rather than the health system. In this new tech world, a phone app seem to be a good option to try. Dr Grainger, in collaboration with her colleagues in RTRU, Hutt Hospital, and the Department of Information Science at University of Otago, first conducted a systematic review of all apps that could enable measurement of RA disease activity by people with RA and for those data to be transmitted to their rheumatology team for monitoring. (This review can be downloaded for free here.) They found the 19 potentially useable app for longitudinal assessment of disease activity,which fell into two categories: 1) simple calculators of disease activity or 2) data tracking tools for people with RA. However, no apps used all the required validated instruments and allowed for data transmission. One high quality app “Arthritis Power” does a great job of longitudinal tracking of validated patient-reported outcomes (PRO’s) and is used for patient-led research but is not suitable for use in “telerheumatology” due to lack of measurement of tender and swollen joints, a key feature of RA activity measured by rheumatologists.
Next steps in this research has been to involve people with RA and rheumatology health professionals to identify required features and functionality of an app for RA disease activity measurement, along with barriers to uptake and advantages of remote monitoring approach. With this information, Dr Grainger’s team has built an app and currently planning how this may be integrated into clinical practice. In parallel with this with, they have also co-designed with people with RA a training package of videos to teach joint count techniques. This will be evaluated in clinics in Wellington, Christchurch and Dunedin in late 2017. Their goal is to enable people with RA to engage in their health care in ways that works for them while still providing appropriate assessment and oversight. Not necessarily “self-management” but “self-led management:”.