Associate Professor Nick Wilson, Dr Nhung Nghiem, Dr Cristina Cleghorn, Professor Tony Blakely
 In this blog post we report on a new study from the BODE3 Programme that suggests that strategies to reduce the dietary salt intake of New Zealanders could produce major health gains and major cost savings for the publicly-funded health sector. We also put these results into a wider context of how nutrition could be improved in NZ.
In this blog post we report on a new study from the BODE3 Programme that suggests that strategies to reduce the dietary salt intake of New Zealanders could produce major health gains and major cost savings for the publicly-funded health sector. We also put these results into a wider context of how nutrition could be improved in NZ.
This study was done given the high importance of dietary sodium (salt) as a global disease risk factor – it is the eleventh most important risk factor globally [1], with the same ranking for Australasia. In particular, we aimed to model the health benefits and costs for NZ of reducing salt intakes – given this is a country that still has a high burden of heart attacks and stroke.
Salt is ubiquitous in processed food, and often at levels that vary widely within the same type of food product eg, different breads. The good news, though, is that salt can be readily reduced by food reformulation – and because people’s taste buds adapt, it is possible to lower salt in food by about 10% a year with virtually no one noticing. Indeed, there is even some research suggesting that when people are on lower sodium diets they may actually prefer them, based on research that measured the hedonic value of dietary sodium [2]. Potassium salts, which are beneficial for health [3], can also be used to replace the sodium in processed foods (which has already been happening to some NZ food such as soups).
In our study, published in the journal PLoS One [4], we modelled reducing sodium in the food supply, but also changes in consumer behaviour eg, via the impact of counselling, food labelling and a UK-style mass media campaign on salt.
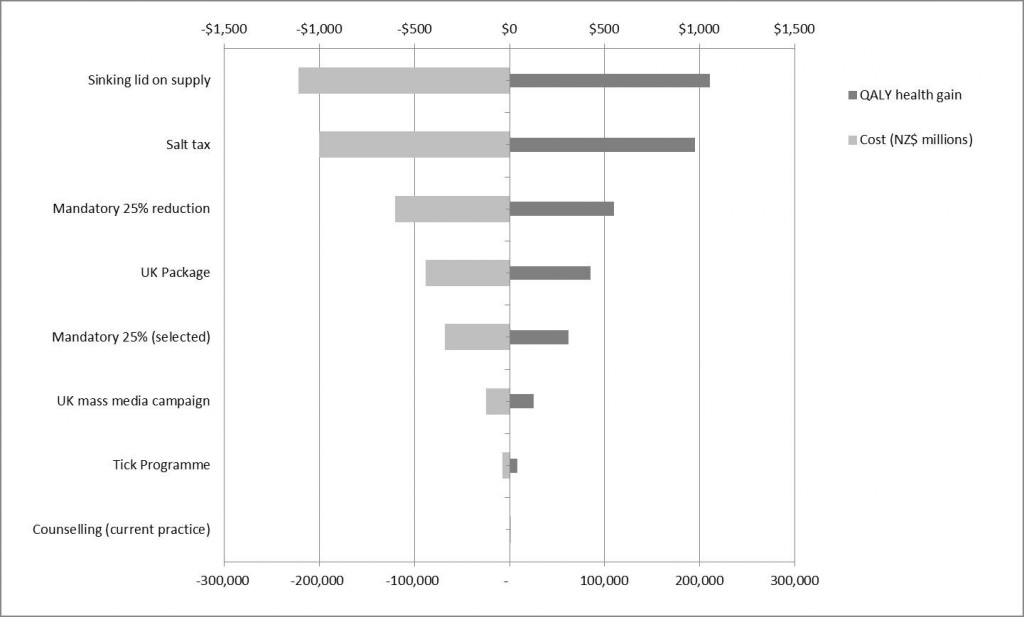
We found that the largest benefit to health (from reducing heart attacks and strokes) came from the strategy of a “sinking lid” on the amount of food salt released to the national market to achieve an average adult intake of 2300 mg of sodium per day. Such an amount compares to around 3500 mg of sodium per day (around 9 grams of salt – or 1.5 teaspoons of salt) currently for the typical NZ adult – mainly from salt hidden in processed foods. This “sinking lid” strategy generated an extra 211,000 quality-adjusted life-years in the adult NZ population alive in 2011 over the remainder of their lifetimes. For many people this will only save days or weeks of life, but for those at risk of heart attacks and strokes in their 50s – the benefit could be measured in decades of extra life. This “sinking lid” strategy resulted in $1.1 billion in cost savings from fewer heart attacks and strokes – even when considering that people would live longer and cost the health system more in their extra life.
The next highest impact strategy was from a salt tax. It also had the advantage of raising revenue which was estimated at reaching about $450 million per year.
Other effective interventions studied were a mandatory 25% reduction in sodium levels in all processed foods and a package of salt reduction strategies performed in the United Kingdom (including a mass media campaign). We also “gave the tick” to NZ’s own “Tick Programme” which is run by the Heart Foundation and was assessed as being a good investment for reducing salt intakes (it is also good for nutrition in other ways: [5]).
Indeed, seven of the eight salt reduction interventions studied generated both health gain for New Zealanders and saved overall health costs. The exception was dietary counselling by dietitians which was found to be good value for the money invested, but just not to the point of actually saving money overall. See the graph below for the key results of all the 8 interventions studied.
Figure: Impact of different interventions to reduce dietary salt intake in the NZ population – showing large health gains and also large financial savings to the health system 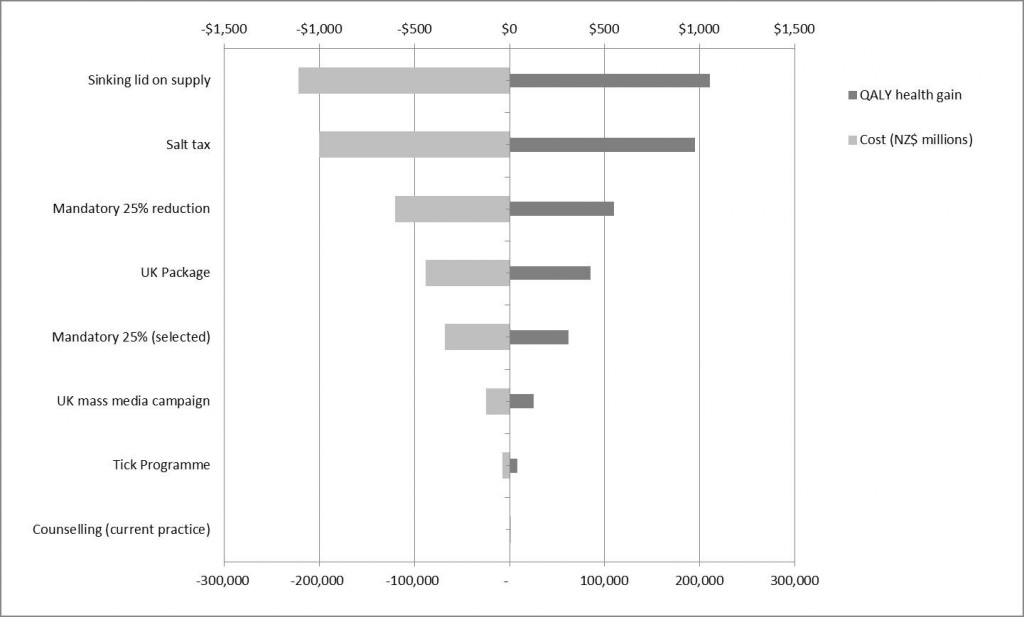 Notes: The mandatory 25% reduction is for the sodium level in all processed foods. For “selected” foods, this is just for bread, processed meats and sauces. QALY: quality-adjusted life-years gained from the intervention (by reducing heart attacks and strokes).
Notes: The mandatory 25% reduction is for the sodium level in all processed foods. For “selected” foods, this is just for bread, processed meats and sauces. QALY: quality-adjusted life-years gained from the intervention (by reducing heart attacks and strokes).
When considered alongside the international literature (which we reviewed in our paper [4]), there were no big surprises in our results. Indeed, there is now a quite large body of evidence that interventions to lower salt intakes are good for population health and are cost-effective. What was new in our study was being able to give results for the NZ population using our own disease and cost data. This work was also able to show that the health gain per person will likely be greater for Maori men and women compared to non-Maori – so salt reduction strategies could help reduce the health gaps.
In terms of the feasibility of introducing these interventions we note that two are already in place in NZ (dietary counselling and the Tick Programme). We also suspect that policymakers may be particularly interested in the other potential interventions as these might be achieved with food industry cooperation – as seen with the past success in reducing salt in bread in NZ.
But while salt reduction strategies would help improve health in adults – there is also an urgent need to tackle adult and child obesity eg, following other countries with a tax on sugar-sweetened beverages (see these two relevant systematic reviews [6], [7] and a meta-analysis [8], our previous publications [9] [10], and past blogs on this topic [eg, here]).
We acknowledged in our new paper that the evidence relating to dietary salt and health is still regarded by some people to be controversial (and we have blogged on this topic previously [eg, here]). But there are some recent publications that strengthen the linkage between salt and increased disease risk – not just heart attacks and stroke but also kidney disease and stomach cancer eg, see: this 2015 review [11]; this 2014 systematic review on the DASH diet [12]; this 2015 systematic review on salt and increased cardiovascular disease mortality [13]; this meta-analysis on stomach cancer risk [14]; and this study on renal cancer risk [15]. There is also growing evidence of damage from dietary salt to blood vessel walls which is separate from the impact on raising blood pressure [16].
We plan to soon publish the results of additional modelling work on salt reduction interventions (including substitution with potassium chloride). We have also been using mathematical modelling to design different types of heart healthy bread – which combines both lower sodium levels with the benefit of higher potassium levels, and other improvements such as higher fibre and levels of omega-3 fatty acids. Such “ideal” bread could be used by government-funded institutions (eg, hospitals) or be promoted via providing healthy bread vouchers for those with existing cardiovascular disease.
The health gains (measured in quality-adjusted life-years) and cost savings reported in this study were all discounted at 3% per annum. For example, $1 earned in 10 years time is worth 74 cents at the current value, in 20 years 54 cents, in 40 years 30 cents, and so on. Such discounting is standard practice in economic analyses. But in scenario analyses in the main paper we also considered no discounting and 6% discount rate.
In summary, there are many potential salt reduction interventions available to NZ policymakers if they wish to take the salt reduction path for achieving health gains and to save health sector costs.
References
- Lim SS, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380(9859):2224-2260.
- Blais CA, et al. Effect of dietary sodium restriction on taste responses to sodium chloride: a longitudinal study. Am J Clin Nutr 1986, 44(2):232-243.
- Peng YG, et al. Effects of salt substitutes on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2014, 100(6):1448-1454.
- Nghiem N, et al. Health and Economic Impacts of Eight Different Dietary Salt Reduction Interventions. PLoS One 2015, 10(4):e0123915.
- Wilson N, et al. Possible impact of the Tick Programme in New Zealand on selected nutrient intakes: Tentative estimates and methodological complexities. N Z Med J 2014, 127(1399):85-88.
- Thow AM, et al. A systematic review of the effectiveness of food taxes and subsidies to improve diets: understanding the recent evidence. Nutr Rev 2014, 72(9):551-565.
- Eyles H, et al. Food pricing strategies, population diets, and non-communicable disease: a systematic review of simulation studies. PLoS Med 2012, 9(12):e1001353.
- Cabrera Escobar MA, et al. Evidence that a tax on sugar sweetened beverages reduces the obesity rate: a meta-analysis. BMC Public Health 2013, 13:1072.
- Ni Mhurchu C, et al. Twenty percent tax on fizzy drinks could save lives and generate millions in revenue for health programmes in New Zealand. N Z Med J 2014, 127(1389):92-95.
- Blakely T, et al. Taxes on sugar-sweetened beverages to curb future obesity and diabetes epidemics. PLoS Med 2014, 11(1):e1001583.
- Farquhar WB, et al. Dietary Sodium and Health: More Than Just Blood Pressure. J Am Coll Cardiol 2015, 65(10):1042-1050.
- Siervo M, et al. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr 2014:1-15.
- Poggio R, et al. Daily sodium consumption and CVD mortality in the general population: systematic review and meta-analysis of prospective studies. Public Health Nutr 2015, 18(4):695-704.
- D’Elia L, et al. Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies. Clin Nutr (Edinburgh, Scotland) 2012, 31(4):489-498.
- Deckers IA, et al. Long-term dietary sodium, potassium and fluid intake; exploring potential novel risk factors for renal cell cancer in the Netherlands Cohort Study on diet and cancer. Br J Cancer 2014, 110(3):797-801.
- Edwards DG, Farquhar WB: Vascular effects of dietary salt. Curr Opin Nephrol Hypertens 2015, 24(1):8-13.