Dr Leah Grout, Prof Nick Wilson, Dr Julie Bennett, Dr Jennifer Summers, Dr Amanda Kvalsvig, Prof Michael Baker *
The importance of indoor aerosol transmission of the virus that causes COVID-19 is increasingly recognised. In addition to public health measures such as masking and physical distancing, further protections are needed to prevent the spread of the virus. Interventions to improve ventilation and filtration are needed for indoor settings in Aotearoa NZ. In this blog we address the particular need to improve ventilation in three settings: (i) homes with contacts who are self-isolating; (ii) indoor workplaces that have essential workers; and (iii) MIQ facilities.
Photo by bady abbas on Unsplash
Introduction
Airborne transmission of the pandemic virus causing COVID-19 has been recognised by the World Health Organization, which states that it can spread in “poorly ventilated and/or crowded indoor settings” [1]. This is also the view of the US Centers for Disease Control and Prevention (CDC), which recommends: “adequate ventilation, and avoidance of crowded indoor spaces” [2]. Moreover, there is confirmation that long-range aerosol transmission (defined as within the same room but more than two metres away) has occurred [3, 4].
Indoor spaces with low levels of ventilation are high-risk settings for transmission, as virus-laden aerosols can remain airborne for hours [3, 5]. A recent review has noted the importance of infectious aerosols as a main way in which Covid-19 has been spread [6]. It notes that droplet transmission alone could not account for the numerous super-spreading events and the differences in transmission between indoor and outdoor environments [6]. To date, ventilation has not been a focus of efforts to reduce transmission in the NZ setting. This is despite the identification of ventilation inadequacies within MIQ facilities (see examples in the appendicised table below).
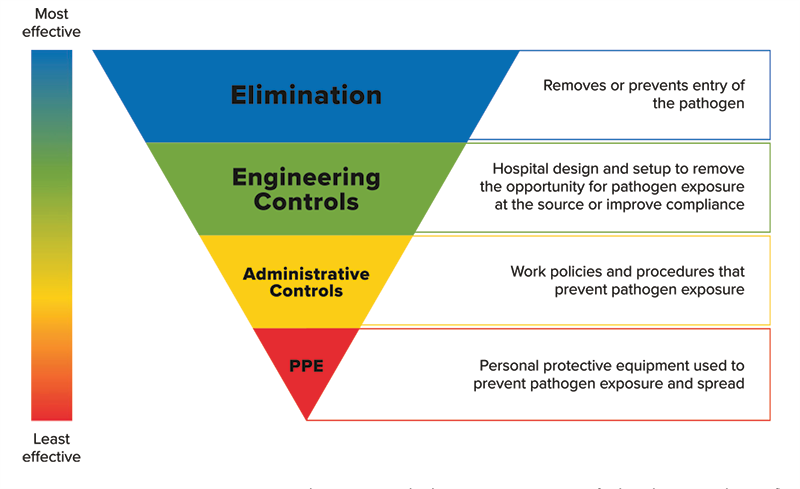
Approaches to preventing exposure to pathogens can be considered in the Hierarchy of Controls for preventing exposure to harmful agents (see Figure 1). While the figure was designed with hospitals in mind, it is relevant for all indoor workplaces during COVID-19 outbreaks. Ensuring adequate ventilation can involve both engineering and administrative controls to reduce exposure to pathogens. These interventions are considered more effective than the use of personal protective equipment (PPE).
Figure 1. Hierarchy of infection control and prevention measures [7].
Modified from: https://www.cdc.gov/niosh/topics/hierarchy/default.html.
Ventilation in homes with contacts who are “self-isolating”
The Ministry of Health website gives advice for those contacts who are “self-isolating” (technically “home quarantine” if they are contacts who have not been diagnosed as cases) [8]. However, in terms of ventilation, this advice is extremely limited with only the words: “keep shared spaces well ventilated”. This advice should be updated to something like the following:
- If possible use a bedroom with at least one window and keep the window(s) open for as much time as possible (outdoor temperature and safety permitting).
- Block any air gaps under the door of the bedroom (eg, with a towel).
- It is particularly important to have the windows open for at least 5 minutes before leaving the bedroom, but then to close the windows just before opening the door to leave the bedroom. The latter is to avoid turbulent air from the bedroom moving into a corridor, as per suggestions made for quarantine facilities [9].
- The person in self-isolation should also open windows when using any shared areas in the house (eg, bathrooms). Generally, the US CDC also recommends using exhaust fans in kitchens or bathrooms, or ceiling fans, to improve airflow and prevent the spread of COVID-19 within homes [10]. However, if a fan is used in the home, then the airflow of the fan should not be directed so that it blows directly from one person towards another person [11].
Such information should also be reiterated when identified contacts call Healthline for advice. Furthermore, the Ministry advice urgently needs upgrading to include the use of masks by people who are self-isolating.
Ventilation in indoor workplaces that have essential workers
Under Alert Level 4 settings there are workers and customers in supermarkets, pharmacies, and healthcare facilities. There are also factories and other workplaces that are in use by essential workers. Generally, experts have advised that to maintain proper ventilation in schools, homes, and businesses to prevent or minimise COVID-19 transmission, building managers should bring in as much outdoor air as possible, with a room air exchange rate of four to six times per hour, which is more than double the rate in a typical office or school building [3, 5]. New Zealand’s pre-pandemic guidelines for schools advised four or more air changes per hour [12], but this advice is not mandated. It has also been recommended that in buildings that recirculate interior air, filters should be upgraded to hospital-grade MERV 13 filters, which can remove up to 70% more small particles (<2.5 microns) than the MERV 8 filters that are typically used [3, 5]. Failing the use of such filters, then window opening is again a very simple approach to improving workplace ventilation.
Requiring mask use by all essential workers who are working indoors under Alert Level 3 and 4 settings would also help to prevent airborne transmission of the virus. Furthermore, there is growing evidence that improved ventilation can result in a range of other benefits in the workplace environment, including improved functioning of workers on cognitive tests, reports of improved sleep, and fewer “sick building” symptoms [13].
There is an urgent need for the Ministry of Health to communicate these ventilation issues to employers, unions, and workers. There is also a need for improved ventilation of schools that are open under Alert Level 3 for children of essential workers, along with mandatory mask wearing by all school children, staff, and school visitors, in line with CDC advice [14].
Ventilation in MIQ facilities
Available evidence indicates that inadequate ventilation has led to multiple quarantine system failures in Australia and NZ [15, 16]. For example, after three transmission events at the Pullman Hotel MIQ facility in Auckland (see appendicised table), it was revealed that corridor ventilation was only operating for two hours per day at the time of the incidents [17]. As a result of the transmission events, a number of changes in the ventilation system and practices were introduced [18]. Short-term changes at the Pullman Hotel included operating at reduced capacity (50%) to reduce congestion in shared spaces, the placement of air purifiers (eg, HEPA units) in the lifts and corridors, expanded use of N95/P2 particulate respirators for MIQ workers (undertaken at all MIQ facilities) [18], and it was also announced that corridor ventilation would operate for 24 hours a day to reduce the risk of airborne transmission [17]. These measures were put into place while longer-term remedial ventilation work was undertaken at the Pullman Hotel [18].
However, the ventilation systems of most hotels used as MIQ facilities are not generally built for quarantine purposes, and a study that examined the ventilation systems in hotels used for quarantine in Hong Kong reported that:
“… it may not be possible to increase the fresh air supply to the hotel premises or install higher-grade filter in the hotel ventilation system. Alternatively, portable air purifiers with HEPA filters should be considered, at least in the corridor of each floor, and ideally in each room. Thirdly, alternate rooms instead of adjacent and opposite rooms should be utilized to reduce the risk of door-to-door transmission. Fourthly, residents are advised to close the windows before opening the doors to avoid unpredicted direction of airflow, and to wear surgical mask for mutual protection while the doors are opened. [9]”
While upgrading ventilation systems and PPE used in hotel-based MIQ facilities may help to prevent/reduce airborne transmission, ideally NZ should move away from the use of hotels to purpose-built quarantine facilities (as being built in Victoria and Queensland), or discrete accommodation units that allow for natural ventilation and reduce or eliminate shared indoor spaces (eg, the cabins used at the Howard Springs facility outside of Darwin, Australia).
In summary, while the country is at Alert Level 3 or 4, efforts should be undertaken to improve ventilation in several different settings in NZ, including: (i) homes with contacts who are “self-isolating”; (ii) indoor workplaces where there are essential workers; and (iii) MIQ facilities. Further work is also needed on ventilation in schools and other settings, and even with improved indoor air ventilation and filtration, other measures including mask wearing and physical distancing will remain important for preventing the spread of COVID-19. Improved indoor air quality will also have health and productivity benefits that extend well beyond the COVID-19 pandemic.
* Author details: Department of Public Health, University of Otago, Wellington
Appendix
Table 1. Examples of confirmed and probable MIQ system failures for COVID-19 control in NZ that may have been related to inadequate ventilation in the facility
| Event | Extent of known spread beyond border | Details |
| Maintenance worker infected in the Rydges Hotel, Auckland MIQ facility (August 2020) | A single worker | A shared lift environment in a quarantine hotel was the source of infection suspected by officials [19], with the sharing occurring only minutes apart [20]. However, officials originally speculated that transmission occurred through touching the same lift button [21]. Genomic sequencing indicated that the case was linked to a recent traveller in the same facility [20]. |
| Traveller-related outbreak linked to the Crowne Plaza, Christchurch MIQ facility (September 2020) | The 2 returnees and 4 others | Three returnees (Cases A, B, and C) tested positive for SARS-CoV-2 while in an MIQ facility (ie, these cases were caught at the border) [22]. Evidence suggests that two returnees (Cases D and E) were then infected through suspended aerosol particles while in the same hotel quarantine facility (Cases D and E were staying in the room next to Case C), before then moving into the community [22, 23]. Transmission from the surface of communal rubbish bins was considered less probable because contact with the bin lid occurred more than 20 hours apart for the involved cases [22]. Furthermore, shared air space is far more likely given what is now known about the likely rarity of transmission via surfaces [24, 25]. The infected returnees appear to have then infected another person (Case G), potentially on a charter flight after leaving the facility [22, 23]. A household contact of Cases D and E was also infected (Case F) [22, 26]. Two household contacts of Case G were also infected [22]. |
| Returnee infectious after leaving the Pullman Hotel, Auckland MIQ facility
“Northland case” (January 2021) |
A single returnee | A returnee was identified as being infectious in the community after leaving a MIQ facility (Pullman, Auckland). The returnee reportedly had the Beta variant (lineage B.1.351) of the pandemic virus [27]. Genome sequencing linked the case to another returnee who was in the same MIQ facility [28]. This might have been part of one single failure at the Pullman facility (ie, a super-spreading event at the facility given the cases in the subsequent two rows of this table). |
| Returnees infectious after leaving the Pullman Hotel, Auckland MIQ facility (January 2021) | 2 returnees and 1 contact | Two returnees (a parent and child) were identified as infectious in the community after being infected with the Beta variant of the pandemic virus with a link to a MIQ facility (Pullman, Auckland) [29]. A close contact (the mother of the child) also became infected [30]. |
| Infection within the Pullman Hotel, Auckland MIQ facility (January 2021) | Contained at the border | A returnee from India via the United Arab Emirates (arrival date 16 January 2021) tested positive on Day 10 in the Pullman MIQ facility in Auckland [31]. Genome sequencing revealed that the case was infected with the Alpha variant (lineage B.1.1.7) of COVID-19 and suggested that this case was closely linked to another case in the facility [32]. The other case in the facility was genomically related to two cases in Australia: one air crew member who tested positive on 13 January 2021 and a subsequent case in a MIQ facility who was on the same flight as the crew member (G. Hall, Ministry of Health, personal communication to Prof David Skegg, 16 March 2021 in response to an OIA request). “Genomic and epidemiological evidence indicate possible transmission within the MIQ” (G. Hall 2021, ibid). Given this evidence and the time frame around first testing positive on Day 10, we would regard this as a “probable” infection within the MIQ facility. |
| Infection within the Grand Mercure Hotel, Auckland MIQ facility (March 2021) | Contained at the border | A returnee in MIQ at Auckland’s Grand Mercure Hotel returned a positive day 12 test [33]. The case travelled from the UK via Singapore [33], but results from genome sequencing showed a link to another case at the Grand Mercure [34]. The two returnees arrived on separate flights within two days of each other, and they were staying in separate rooms on different floors [34]. |
| Infection within the Jet Park Hotel, Auckland MIQ facility (July 2021) | Contained at the border | A bubble of 3 people in the Jet Park Hotel tested positive for Covid-19 in July and the cases were genomically linked to a COVID-19 case in the room opposite [35, 36]. The Auckland Regional Public Health Service investigation found that doors to rooms on opposite sides of the corridor were opened at the same time for about three to five seconds on four occasions between July 27 and July 29, while the case in the room opposite was infectious [35, 36]. |
| Delta variant infection within the Crowne Plaza, Auckland MIQ facility (August 2021)
|
Related to Auckland Delta outbreak | A bubble of three people in the Crowne Plaza returned a positive day 12 test on 18 August. These returnees were in a room adjacent to the primary case from NSW in the current Auckland outbreak [37]. |
References
- World Health Organization. Coronavirus disease (COVID-19): How is it transmitted? Geneva, Switzerland 2020 [updated 30 April 2021]. Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted.
- CDC. SARS-CoV-2 Transmission US Department of Health & Human Services; 2021 [updated 7 May 2021]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html.
- Allen JG, Ibrahim AM. Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission. JAMA. 2021; 325(20): 2112-3. DOI: 10.1001/jama.2021.5053.
- National Academies of Sciences, Engineering, and Medicine. Airborne Transmission of SARS-CoV-2: Proceedings of a Workshop – in Brief. Washington, DC: The National Academies Press; 2020. Available from: https://www.nap.edu/catalog/25958/airborne-transmission-of-sars-cov-2-proceedings-of-a-workshop.
- The Lancet COVID-19 Commission Task Force on Safe Work, Safe School, and Safe Travel. Six Priority Areas. 2021. Available from: https://static1.squarespace.com/static/5ef3652ab722df11fcb2ba5d/t/60a3d6713c9af62b4c2037ff/1621350002802/Safe+Work%2C+Safe+School%2C+Safe+Travel+%28Feb+2021%29.pdf
- Wang CC, Prather KA, Sznitman J, et al. Airborne transmission of respiratory viruses. Science. 2021; 373(6558): eabd9149. DOI: 10.1126/science.abd9149.
- American Animal Hospital Association. Infection control strategies 2021. Available from: https://www.aaha.org/aaha-guidelines/infection-control-configuration/infection-control-strategies.
- Ministry of Health. COVID-19: Self-isolation, managed isolation/quarantine 2021 [updated 22 August 2021]. Available from: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-health-advice-public/covid-19-self-isolation-managed-isolation-quarantine.
- Wong SC, Chen H, Lung DC, et al. To prevent SARS-CoV-2 transmission in designated quarantine hotel for travelers: Is the ventilation system a concern? Indoor Air. 2021; 31(5): 1295-7. DOI: 10.1111/ina.12870.
- CDC. Improving Ventilation in Your Home 2021 [updated 7 January 2021]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/Improving-Ventilation-Home.html.
- EPA. Indoor Air in Homes and Coronavirus (COVID-19): United States Environmental Protection Agency; 2021 [updated 16 July 2021]. Available from: https://www.epa.gov/coronavirus/indoor-air-homes-and-coronavirus-covid-19.
- Ministry of Education. Designing Quality Learning Spaces: Indoor Air Quality and Thermal Comfort – Version 1.0, September 2017. 2017. Available from: https://www.education.govt.nz/assets/Documents/Primary-Secondary/Property/Design/Flexible-learning-spaces/DQLSIndoorAirQualityThermalComfortV1-0.pdf.
- Starr D. The air investigator. Science. 2021; 373(6555): 612-5. DOI: 10.1126/science.373.6555.612.
- CDC. COVID-19: Schools and Child Care – K-12 Schools 2021 [updated 5 August 2021]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html#.
- Grout L, Katar A, Ait Ouakrim D, et al. Estimating the failure risk of quarantine systems for preventing COVID-10 outbreaks in Australia and New Zealand. Med J Aust. 2021; https://www.mja.com.au/journal/2021/estimating-failure-risk-quarantine-systems-preventing-covid-19-outbreaks-australia-and [Preprint, 9 July 2021].
- Grout L, Katar A, Summers J, et al. Australia’s Quarantine Systems Failures: Lessons for NZ. University of Otago, New Zealand 2021. Available from: https://blogs.otago.ac.nz/pubhealthexpert/australias-quarantine-systems-failures-lessons-for-nz/.
- Covid19 coronavirus: How three returnees caught virus at Pullman Hotel. New Zealand Herald. 2021 (16 February); Sect. New Zealand. Available from: https://www.nzherald.co.nz/nz/covid-19-coronavirus-how-three-returnees-caught-virus-at-pullman-hotel/PBC22AJTEKXBJ7TLZUCXNKUZOI/.
- Ministry of Business Innovation & Employment. Pullman MIQ facility to reopen to full capacity following report release [press release]. New Zealand, 23 April 2021. Available from: https://www.miq.govt.nz/about/news/pullman-miq-facility-to-reopen-to-full-capacity-following-report-release/
- Ministry of Health. 1 case of COVID-19 in quarantine worker [press release]. New Zealand, 7 November 2020. Available from: https://www.health.govt.nz/news-media/media-releases/1-case-covid-19-quarantine-worker
- Hadfield J, Douglas J, Geoghegan J, et al. Re-emergence of community transmission in Aotearoa New Zealand – Genomic overview of the Auckland Outbreak. (Accessed 28 October 2020). ESR. https://nextstrain.org/community/narratives/ESR-NZ/GenomicsNarrativeSARSCoV2/2020-10-01?n=5.
- Leahy B. Covid19 coronavirus: Rydges Hotel worker may have caught virus using a lift. New Zealand Herald. 2020 (20 August). Available from: https://www.nzherald.co.nz/nz/covid-19-coronavirus-rydges-hotel-worker-may-have-caught-virus-using-a-lift/ECOIYGF3V4UY4FJGU2QIKJD3NQ/.
- Eichler N, Thornley C, Swadi T, et al. Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 during Border Quarantine and Air Travel, New Zealand (Aotearoa). Emerg Infect Dis. 2021; 27(5). DOI: 10.3201/eid2705.210514.
- Ministry of Health. No new cases of COVID-19 [press release]. New Zealand, 2 October 2020. Available from: https://www.health.govt.nz/news-media/media-releases/no-new-cases-covid-19-50
- Lewis D. COVID-19 rarely spreads through surfaces. So why are we still deep cleaning? Nature. 2021; (E-publication 29 January). https://www.nature.com/articles/d41586-021-00251-4.
- Meyerowitz EA, Richterman A, Gandhi RT, et al. Transmission of SARS-CoV-2: A Review of Viral, Host, and Environmental Factors. Ann Intern Med. 2021; 174(1): 69-79. DOI: 10.7326/M20-5008.
- Ministry of Health. 2 new cases of COVID-19 [press release]. New Zealand, 27 September 2020. Available from: https://www.health.govt.nz/news-media/media-releases/2-new-cases-covid-19-21
- Ministry of Health. 2 cases of COVID-19 in managed isolation; update on Northland case [press release]. New Zealand, 26 January 2021. Available from: https://www.health.govt.nz/news-media/media-releases/2-cases-covid-19-managed-isolation-update-northland-case
- Ministry of Health. Update on Northland case, and 6 cases of COVID-19 in managed isolation [press release]. New Zealand, 25 January 2021. Available from: https://www.health.govt.nz/news-media/media-releases/update-northland-case-and-6-cases-covid-19-managed-isolation
- Ministry of Health. 3 new cases of COVID-19 at the border and an update on border-related cases in Auckland [press release]. New Zealand, 28 January 2021. Available from: https://www.health.govt.nz/news-media/media-releases/3-new-cases-covid-19-border-and-update-border-related-cases-auckland
- Ministry of Health. 7 cases of COVID-19 [press release]. New Zealand, 4 February 2021. Available from: https://www.health.govt.nz/news-media/media-releases/7-cases-covid-19
- Ministry of Health. 4 new cases of COVID-19 in managed isolation; 1 historical case [press release]. New Zealand, 27 January 2021. Available from: https://www.health.govt.nz/news-media/media-releases/4-new-cases-covid-19-managed-isolation-1-historical-case
- Ministry of Health. 4 cases of COVID-19 in managed isolation [press release]. New Zealand, 2 February 2021. Available from: https://www.health.govt.nz/news-media/media-releases/4-cases-covid-19-managed-isolation-0
- Nichols L. Covid 19 coronavirus: Officials investigating if positive MIQ case caught virus from another guest. New Zealand Herald. 2021 (22 March); Sect. New Zealand. Available from: https://www.nzherald.co.nz/nz/covid-19-coronavirus-officials-investigating-if-positive-miq-case-caught-virus-from-another-guest/UDW4MLSP3ONM34WUPMM5I6OLJA/.
- Ministry of Health. No new community cases; 6 cases of COVID-19 in managed isolation [press release]. New Zealand, 25 March 2021. Available from: https://www.health.govt.nz/news-media/media-releases/no-new-community-cases-6-cases-covid-19-managed-isolation-0
- Small Z. COVID-19 transmission at Auckland’s Jet Park quarantine facility likely from room doors being opened simultaneously. Newshub. 2021 (17 August). Available from: https://www.newshub.co.nz/home/politics/2021/08/covid-19-transmission-confirmed-at-auckland-s-jet-park-quarantine-facility-from-room-doors-being-opened-simultaneously.html.
- Ministry of Business Innovation & Employment, Ministry of Health. Low risk in-facility transmission confirmed at Jet Park MIQ facility [press release]. New Zealand, 17 August 2021. Available from: https://www.health.govt.nz/news-media/media-releases/low-risk-facility-transmission-confirmed-jet-park-miq-facility
- Ministry of Health. 11 additional community cases; 6 new cases and 2 historical cases in managed isolation facilities [press release]. New Zealand, 19 August 2021. Available from: https://www.health.govt.nz/news-media/media-releases/11-additional-community-cases-6-new-cases-and-2-historical-cases-managed-isolation-facilities



could better ventilation result in people passing on the viruses to their neighbours especially for people living in apartment blocks or who live very close to their neighbours?
The point is that the virus needs to build up in the air, to a concentration at which the inoculum dose inhaled by someone else, will make them ill. If the air is moving, and carrying viruses into the outdoors, ventilation means “de risking”, not increased risk.
These Dutch authors have made in interesting attempt at a simple but lengthy (of necessity) explanation of how aerosol infection works, what are the factors:
https://www.maurice.nl/2021/09/26/covid-19-de-moeizame-weg-van-mens-tot-mens/
Google Translate works well for me.
I particularly like this para:
“…outside has no effect whatsoever, the dilution of the exhaled air goes so fast that it is impossible that enough virus remains around a susceptible person to infect that person. It is statistically impossible for it to happen…”
There is a summarized version linked at the end.
This is encouraging news. At last. Here is a great video from Dutch TV where an aerosol spread expert tells his side of the story in October 2020:
https://www.youtube.com/watch?v=tJSPL9LQCiM
As Prof. Jimenez (UColorado, Boulder) implies, it is a pity the WHO’s inertia has prevented people from taking mitigation precautions at a high level of benefit-cost for well over a year. The mandated mitigation precautions have had very high cost.
Reducing the aerosol risk in rest homes surely has to be the MOST important thing, yet you don’t mention it! The fact that rest home deaths are so much higher than deaths among the same-aged independently-living was one clue among many that aerosol spread was the problem. Higher rates of air exchange in these environments is essential, and financial assistance should be provided by government for the resulting higher costs of heating cold air. Residents should be encouraged to socialize outdoors – locking rest home residents indoors for prolonged periods with no attention to ventilation has certainly in many parts of the world, killed people rather than saved them.
Your advice about isolated and quarantined people needing fresh air will also avert a similar situation where people have in many parts of the world, been killed by a buildup of their own viruses in a small unventilated space in which they were dutifully confining themselves.
It should also be obvious that the path of this virus into rest homes even under lockdown conditions, is via staff who share housing space with infected people who are not yet caught up with by contact tracing. Rest home staff living in crowded rental accommodation are obviously a higher risk than those living in housing with more indoors space. Unfortunately, a lockdown immediately increases the chance of infection between these people, due to the buildup of aerosol virus being enabled for a much higher proportion of the time than would be the case when people are coming and going and keeping out of each other’s faces as much as possible (a norm in crowded rental accommodation).
We are on a knife-edge of risk of outbreaks in the most deadly environments. And in the long term there could be new viruses that spread the same way, and your Hierarchy of infection prevention and control measures is especially appropriate. “Energy efficiency” policy has possibly been taking us in the wrong direction for indoor environment health and we need to reverse this. 2020 may be “peak sick building syndrome” as much as it was anything else.
One last minor point: aerosols shed from damp fabric as it is drying out, so masks dropped into open-topped rubbish bins or merely left lying around, may be one source of aerosols that has not yet been identified.
Further to the comment I already made – are the authors urgently advocating for this essential advice to be applied to the conditions in which increasing numbers of people in the community who test positive are being confined? Even if the intentions are there to follow this advice, the ad-hoc nature of provisions to confine increasing numbers of people without sufficient prior allocation of resources to ensure safety could have tragic consequences. Is there any notice being served on those responsible, that severity of illness may we worsened, and even death that was otherwise avoidable may result? Of course every case of avoidable worsened illness that has to be moved to hospital is an “own goal”.
Almost anything would be a lesser evil than hastily improvised use of poorly ventilated buildings, and any crowding associated with the process.