Amanda D’Souza, Nikki Turner*
This blog is part of the Public Health Solutions series looking at effective public health measures to reduce demand on healthcare quickly. This blog looks at solutions to improve child health: a child impact lens on policy, lifting income support, action on childhood immunisation.
Image by Luke Pilkinton-Ching, University of Otago
Childhood provides essential foundations for lifelong health. However even before the COVID-19 pandemic, Aotearoa’s health system struggled with persistently high rates of preventable hospitalisations, ill-health, and large health inequities among children and young people. This is because of unacceptably high rates of child poverty, inadequate household income, and poor housing, leading to under-nutrition, recurrent illness, and high levels of stress among whānau. Tamariki Māori and Pasifika children are particularly disadvantaged by the impacts of institutional racism and service systems that do not fully reflect Te Tiriti o Waitangi obligations or Aotearoa’s cultural diversity.
Unfortunately, the direct and indirect impacts of the pandemic have worsened the situation for many children and whānau and placed even more pressure on a health system. This pressure makes it challenging for the health system to be geared towards child wellbeing and preventive health. A key task for policy-makers is for Aotearoa to make a genuine shift in approach so that all children can thrive.
This blog highlights three important interventions to implement quickly to improve child wellbeing and alleviate the pressures on our health system.
- Child Impact Lens: This is a routine assessment on all policies that impact on children. It is intended to ensure that the best interests of children are primary considerations in all policy decisions that impact children and young people. Extensive guidance is available for organisations to action existing duties to children and whānau under the UN Convention on the Rights of the Child (UNCRC). All organisations should be aware of and resourced to implement UNCRC, including routinely assessing with a child impact lens all key policy changes and service developments that have a direct or indirect effect on children’s lives.
- Lift income support rates for children in greatest hardship, including core benefits for children and carers: The level of income support available to large numbers of carers and whānau with children, especially those with additional needs, is currently too low to provide a strong foundation for healthy development. Children need adequate living standards to enable food security for good nutrition, healthy and secure housing, participation in society, and for carers and whānau to have sufficient resources and capacity for parenting. While current government initiatives** are welcome, household incomes are still inadequate for children in the greatest poverty. Depending on which measure is chosen, over 180,000 children live in households with inadequate income and over 125,000 experience material hardship.
- Sustained action to achieve high and equitable coverage of childhood immunisations: Internationally, concerns are escalating about deteriorating childhood immunisation coverage since the pandemic, highlighted by recent cases of rare/eradicated infections such as polio (USA) and diphtheria (Australia). A local outbreak of measles in 2019 (due to low immunisation rates in the 1980s and 90s) resulted in over 1500 confirmed measles cases and over 500 hospitalisations, especially impacting on Māori and Pasifika communities. Tragically, the epidemic spread to Samoa with 83 lives lost. In Aotearoa, in the decade before the pandemic, immunisation coverage increased from a low base through a multi-pronged approach. Large inequities in immunisation for tamariki Māori and Pasifika children were also narrowing over this time. Vaccine coverage for Māori started to drop in 2017/2018, with larger declines during the pandemic (see Figure 1 below). Health services are working hard to improve these falling rates of routine immunisations despite major health reforms and sector fatigue. The challenge for government is to sustain the focus and learn the lessons from COVID-19 vaccine delivery. In particular, to properly and sustainably resource the health sector and Māori and Pasifika communities to achieve equitable coverage over the long-run.
Figure 1 Immunisation coverage at 24 months of age, by ethnicity (Jan 2016 to June 2022)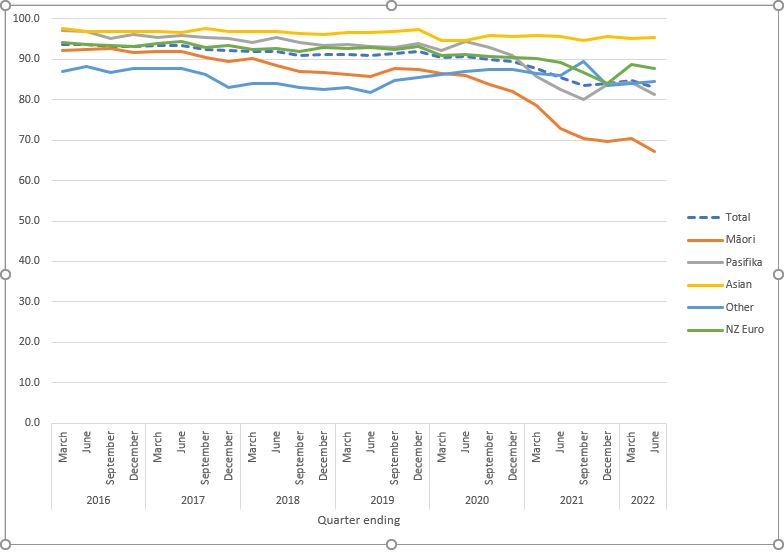
Source: Immunisation Advisory Centre, based on data from the National Immunisation Register, Ministry of Health.
Other evidence-based interventions to prevent child ill-health and inequities might need law changes and take time (although recent developments in folic acid fortification, water fluoridation, and smoke-free legislation shows that with focus, relatively fast change is possible). Urgent work is now needed to obtain cross-party support to enact laws protecting children and whānau from the rampant commercial exposure to junk foods, sugary drinks, and alcohol.
**Such as measuring and tracking child poverty, the Best Start/winter energy payments, and increased Family Tax Credits.
* Author details: Amanda D’Souza is a member of the Department of Public Health, University of Otago Wellington. Nikki Turner works for IMAC (the Immunisation Advisory Centre) and the University of Auckland.



Superb work Amanda and Nikki. Succinct policy advice with relevant public health measures that can quickly improve children’s health and wellbeing and reduce demand on health systems.