Prof Michael Baker, Dr Jennifer Summers, Dr Amanda Kvalsvig, Dr Matire Harwood, Prof Nick Wilson*
In this blog we summarise how Aotearoa New Zealand (NZ) could improve preparations for a likely national outbreak of the Omicron variant of SARS-CoV-2 to minimise harms to health and the economy. The first urgent priority is to increase measures to delay the arrival of the Omicron variant to give more preparation time. We also need to consider an explicit shift from the current suppression strategy to mitigation. A clear mitigation strategy will favour adjustments to existing public health and social measures to ‘flatten the curve’ and minimise the risk of health service overload and social and economic disruptions.
Photo by Luke Pilkinton-Ching, University of Otago Wellington
Updated threat assessment from Omicron and Delta variants
In this blog we update the commentary from our pre-Christmas blog about the need for maximum preparation for a likely national outbreak arising from importing the Omicron variant of SARS-CoV-2, while at the same time continuing to suppress (and perhaps even eliminate) the circulating Delta variant in NZ.
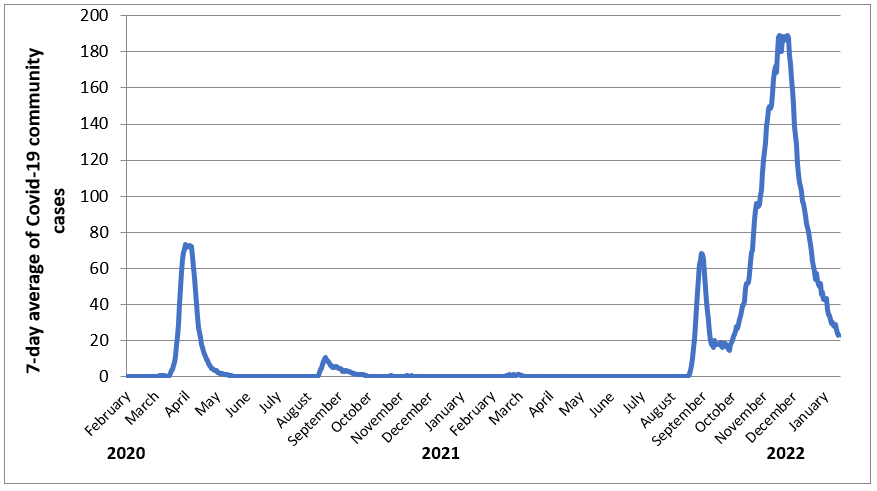
Since reaching a peak of around 200 community cases a day in mid-November 2021, Delta cases have continued to decline to around 30 cases a day (Figure 1). This decline is also reflected in hospitalised cases (and to a lesser extent cases in ICU) providing strong support that this is a real decline in incidence as opposed to changes in case detection (Figure 2).
Figure 1: New Zealand’s 7-day average of Covid-19 cases in the community (confirmed and probable) (from 1 February 2020 to 16 January 2022 from Ministry of Health data)
Figure 2: New Zealand’s 7-day average of Covid-19 hospitalisations and cases in ICU or HDU (from 1 August 2021 to 16 January 2022 from Ministry of Health data on daily cases in hospital and ICU (Intensive Care Unit) or HDU (High Dependency Unit))
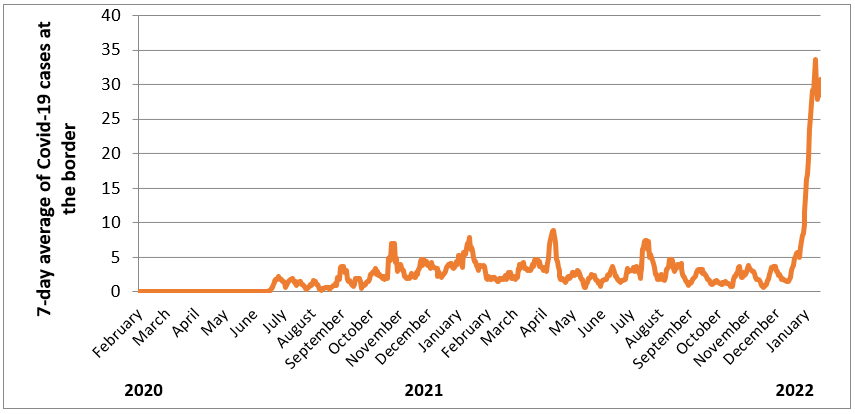
By contrast, the threat of an Omicron outbreak in NZ has increased markedly. NZ is seeing a huge increase in cases being detected at the border and in MIQ (Figure 3). We have now had two known case introductions (including a household contact of an Air New Zealand crew member and a confirmed case in an MIQ border worker) but have so far avoided sustained local transmission.
Figure 3: New Zealand’s 7-day average of Covid-19 cases at the border (from 1 February 2020 to 16 January 2022 from Ministry of Health data on daily MIQ (Managed Isolation and Quarantine) cases)
We are also learning more about the impact of the Omicron variant on population health from observing this variant spreading internationally and from laboratory and other scientific studies. This evidence is suggesting that Omicron typically causes less severe illness than Delta, but overall it should still not be considered a mild infection.
This Omicron variant is also far more transmissible than previous variants. Much of this capacity comes from substantial immune evasion properties. It also has a shorter median incubation period of 3 days. Consequently, it is causing explosive outbreaks in many countries and in indigenous communities. A recent WHO estimate was that it would infect half of the population of Europe (around 374 million) in the next two months. Therefore, a poorly controlled Omicron outbreak in NZ risks overwhelming the health care system, increasing inequities, and disrupting essential services as is being seen overseas.
The experience of Australia probably provides the best example of what NZ can expect to see, given that its population immunity has largely come from vaccination rather than previous uncontrolled waves of infection and vaccination coverage is similarly high to NZ. Their pandemic waves, mainly driven by Omicron, now appear to be peaking in NSW and Victoria. They are also showing that Covid-19 hospitalisations and deaths are largely uncoupled from these huge waves of infection but they are still occurring in relatively high numbers, putting severe strain on health care capacity in Australia and other essential services.
The good news is that some countries are now emerging from Omicron outbreaks which resulted in far fewer deaths than previous outbreak waves. A notable example is South Africa which is now relaxing restrictions.
Photo by Roger Starnes Sr on Unsplash
Urgent actions to minimise harms from the Omicron variant
Act urgently to delay the entry of Omicron: There are multiple benefits in NZ delaying the entry of Omicron to give us more time to prepare for this virus. The revised border opening schedule announced on 21 December means that the “Phased border re-opening is being pushed out to the end of February”, but this timing is too early in our view.
To provide a higher chance of delaying the entry of Omicron, it will be necessary to greatly reduce the number of infected travellers arriving in NZ. Analysis of previous border failures indicates a failure occurring every 100-200 cases in MIQ [1], although this risk estimate will be a bit different now with changes in MIQ worker and traveller vaccination levels and the more infectious nature of Omicron. While not all of these failures will result in a community outbreak, a certain proportion almost certainly will.
The number one priority should be taking rapid action to ‘turn down the tap’ on the number of infected cases arriving in NZ, as this country has done before. That means doing a risk analysis of where the cases are coming from, and if we’re getting more than a certain proportion from some source countries, limiting travel from them until conditions change. If we can push the number of active border cases down to a more manageable number (eg, less than five a day) then we’ve got a much better chance of delaying Omicron’s arrival.
NZ also needs to urgently tighten pre-departure testing requirements. These were recently relaxed by expanding the list of countries where PCR testing was no longer mandatory and a rapid antigen test (RAT) could be used instead. That list now includes Australia, presumably for pragmatic reasons. One option would be to add in a requirement for RAT at overseas airports immediately prior to departure alongside the current PCR requirement 48 hours prior to departure.
Continue suppressing and ideally eliminating the Delta variant outbreak in NZ: The continuing decline in Delta variant cases in NZ, and the stamping out of outbreaks in many parts of NZ, suggests that elimination of this variant is technically possible. Elimination of Delta would put NZ in a better position if it could be achieved before Omicron starts to circulate widely in NZ.
Achieving that goal would require additional effort eg, making much greater use of MIQ facilities to isolate Delta cases rather than relying on home isolation. For any cases still isolating at home, there could be more intensive support provided by health, whānau ora, and welfare authorities/community groups along with better quality and well-fitted masks.
Continue to boost population immunity to Omicron (and Delta): One of the main reasons to delay the entry of Omicron is to allow more time for delivering the ‘booster’ 3rd dose of the vaccine for the vaccinated 18+ age-group. This booster provides relatively good protection against infection from both Omicron and Delta. Analysis of data in the UK found that people who are boosted are up to 92% less likely to be hospitalised with Omicron compared with unvaccinated people. Delaying entry of Omicron also allows for the vaccination of a maximum number of 5-11-year-olds.
Vaccination is particularly important in NZ because there has been minimal exposure to widespread circulating virus. By contrast, in the UK which has high vaccine coverage, high booster uptake, and almost 2-years of exposure to circulating virus, about 97-98% of adults test positive for SARS-CoV-2 antibodies.
The roll-out of boosters and vaccination of children is a particularly important opportunity to prioritise delivery to Māori, Pasifika, those with underlying illnesses, and other at-risk populations such as those in aged-care residential facilities.
Shift to a mitigation strategy to slow the spread of Omicron: Once Omicron arrives in the NZ community, the Government should consider an immediate shift in its Covid-19 strategy (see here for strategy definitions:[2]). That is, it should shift from its current suppression to a mitigation strategy (just as it shifted from elimination of earlier variants to tight suppression of Delta[3]). This would be an explicit recognition that Omicron outbreaks are extremely hard to eliminate or substantially suppress, and so the best that can be feasibly achieved in the NZ setting is to mitigate spread so as to minimise harm in the most vulnerable, to prevent the health system being overwhelmed, and to reduce social and economic disruption.
As a result, the primary focus moves from minimising the number of infections to a ‘flatten the curve’ goal. The mitigation strategy is a central feature of the New Zealand Influenza Pandemic Plan (NZ’s current pandemic plan) which has the stated key objective: “To minimise deaths, serious illness and serious disruption to communities and the economy arising from an influenza pandemic.”
Introduce an upgraded Alert Level system: Based on experience in comparable countries, we can expect an Omicron outbreak to be very intense. To ‘flatten the curve’ may need a brief period of controls that are equivalent to components of the previously used Alert Level system.
The traffic light system is largely orientated towards achieving an indoor vaccine mandate. This system is now less effective since the vaccine passes are based on people being double vaccinated rather than having a booster as well. This limitation could be fixed in time but ultimately the traffic light system lacks an adequate range of tools. Furthermore, contact tracing will be rapidly overwhelmed in an Omicron outbreak and soon become ineffective. This leaves public health and social measures (such as mask use, indoor ventilation, a strengthened sick leave system, a ‘stay at home order’ for non-essential workers, limits on high risk settings such as bars and nightclubs, and stringent measures to reduce transmission in schools) as the main tools to ‘flatten the curve’ of the outbreak. These measures now have a much stronger empirical base. Consequently, the Government urgently needs to consider introducing a revised alert level system, potentially along the lines that we have previously described [4].
Develop and implement an Aotearoa NZ mask strategy: NZ needs a well-developed mask strategy to support the effective use of high-quality masks in all settings where they will make a meaningful difference. Masks are effective against all Covid-19 variants, so are needed to help to ‘flatten the curve’ in the event of an Omicron outbreak. A strategy is needed to ensure high availability and uptake, particularly indoors. There is increasing international advice that people should shift to using higher quality N95 respirator style masks routinely when indoors with other people during an Omicron outbreak. Although these masks are ‘disposable’, each can be worn multiple times. This strategy will require Government action to ensure adequate supply, universal affordability, and suitable quality standards.
Support schools, workplaces, and essential services to prepare for Omicron: There are multiple ways that schools, workplaces and essential services can prepare for the arrival of Omicron. These measures include vaccination (and vaccine mandates for all essential industries), adequate sick leave policies, social support, cohorting, ventilation and filtration of indoor air, and mask use policies to minimise transmission in indoor environments. Children’s health and wellbeing must be supported whether they are accessing in-school or home learning. Active preparation for Omicron will support children and educators and help to ensure that children’s environments are as safe as possible.
Upgrade Covid-19 testing capacity: It is clear from overseas experience that the role of testing will change markedly during an intense Omicron outbreak where it could have an important role in helping to ‘flatten the curve’ and support the care of infected people at home. This is very different to the role of testing as part of contact tracing where highly accurate PCR testing has been critical in identifying infected people as part of the elimination and suppression strategies. Nevertheless, PCR testing will still be important, particularly in the hospital setting.
There is an increasingly important role for rapid antigen tests (RATs) which have been introduced into NZ for a limited range of purposes. In an Omicron outbreak these tests would be valuable to support members of the public to confirm that they are likely to be infectious, and to support them to isolate and inform their contacts. They are also useful for screening asymptomatic people prior to them attending essential work, school, or other settings where they will have contact with others. As with all tests, it is vital to ensure that they are introduced in a way that supports better decision-making and equity. There are many potential problems to avoid. One added requirement is to provide a system that allows members of the public to upload the results of RATs to support ongoing disease surveillance (including both positive and negative results as is the case in parts of Australia).
Protect the healthcare system and provide support for home care: Overseas experience suggests that the great majority of people with illness from Omicron can be cared for at home, which will take some pressure off the hospital system. The public will need practical advice and support about how to manage with Covid-19 infection at home, as appropriate. This advice will need to cover such areas as: Recognising when they are seriously sick and need to get additional help or call an ambulance (ie, especially for those with pre-existing conditions); Essential supplies they should have including pharmaceuticals to manage symptoms; Guidance to minimise transmission in the household, if there are other people living there; and Arrangements for others to check on them if they get sick at home, particularly if living alone.
Other measures to reduce hospital demand include being able to suspend elective surgery at the right time and to reduce hospitalisations from potentially preventable injuries and illness (eg, temporarily lowering traffic speed limits and blood alcohol limits; re-energising our current childhood immunisation programme to achieve rates >95%; promoting innovation in the areas of mental and chronic health-conditions).
NZ may also need to review its isolation requirements for infected and exposed healthcare workers if healthcare services are threatened by worker shortages, as has been done overseas.
Longer term measures to reduce the risk from new variants
Two years of experience managing Covid-19 suggests we should plan for the possibility of a continuing succession of new variants which spread because of their ability to evade the immune protection offered by previous infections and vaccines. We are fortunate that the Omicron variant appears to be less severe than the Delta variant. As evolutionary biologists remind us, there is no guarantee that this process will produce further variants that are less virulent, or that Covid-19 will become endemic.
NZ like other jurisdictions needs to continue building its capacity for high-quality risk assessment and management so that it can adapt its response strategy to changes in the pandemic. Key principles will continue to include: science-informed strategic leadership; a Tiriti and equity focus; use of the precautionary principle; and the need to create legacy benefits for our healthcare and public health systems [3].
Reducing the generation of new variants of concern will be supported by measures to minimise circulation of SARS-CoV-2 at the global level. That goal depends on improved global health leadership and equity to delivery vaccines and other interventions [5].
* Author details: MB, JS, AK, NW are with the Department of Public Health, University of Otago Wellington. MH is at the Department of General Practice and Primary Care, University of Auckland and also a GP at Papakura Marae.
References
- Grout, L., et al., Failures of quarantine systems for preventing COVID-19 outbreaks in Australia and New Zealand. Med J Aust, 2021. 215(7): p. 320-324.
- Baker, M.G., N. Wilson, and T. Blakely, Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. BMJ, 2020. 371: p. m4907.
- Baker, M.G., et al., The next phase in Aotearoa New Zealand’s COVID-19 response: a tight suppression strategy may be the best option. N Z Med J, 2021. 134(1546): p. 8-16.
- Kvalsvig, A., et al., Expansion of a national Covid-19 alert level system to improve population health and uphold the values of Indigenous peoples. Lancet Reg Health West Pac, 2021. 12: p. 100206.
- Sirleaf, E.J. and H. Clark, Report of the Independent Panel for Pandemic Preparedness and Response: making COVID-19 the last pandemic. The Lancet, 2021.




All seems sensible to me in this Blog. Only one comment/suggestion – is it wise to delay Omicron as long as possible? Yu want NZ at ‘peak immunity’ when Omicron gets in. That is a function of HOW LONG since each person was double vacc or boosted. To exaggerate, if everyone was boosted in NZ tomorrow, then you have peak immunity in 14 days – and that is when you want Omicron to come in, not later. Moreover, in reality it takes time for Omicron to build up a head of steam (say 4 to 6 weeks) – you want peak immunity 4-6 weeks after Omicron starts. I do not have the exact answer for this, just suggesting that delaying as long as possible may not be ideal – and timing matters and is something NZ has that we did not on the east coast of Aust. Best, Tony
An excellent article which is science based. I hope the Government accepts your advice.