Dr Ian Longley and Dr Julie Bennett*
Poor ventilation in indoor settings is widely recognised as a risk factor for the airborne transmission of the virus (SARS-CoV-2) that causes Covid-19. Virus-laden aerosols can remain airborne for hours in indoor spaces with low levels of ventilation. In this blog, we discuss how to use carbon dioxide (CO2) measures as a proxy for estimating the level of ventilation in a building and to guide ventilation improvements in schools and workplaces.
Photo by RODNAE Productions from Pexels
Airborne transmission of the virus (SARS-CoV-2) causing Covid-19 has been recognised by the World Health Organization, which states that the virus can spread in “poorly ventilated and/or crowded indoor settings”. This is also the case with the US Centers for Disease Control and Prevention (CDC), which recommends: “adequate ventilation and avoidance of crowded indoor spaces”.
Airborne transmission differs from the traditional view that respiratory viruses either spread through large respiratory droplets (face-to-face), or contact with contaminated surfaces (fomite transmission) [1]. While droplets fall to the ground, aerosols can float in the air for hours, accumulating over time in poorly ventilated spaces [2]. Public health measures such as physical distancing and disinfection are not able to provide adequate protection against airborne transmission. One way to reduce the potential viral dose that can be inhaled is to increase ventilation to help disperse viral particles [3].
What is ventilation?
Ventilation simply means the replacement of contaminated or stale air with clean air. Outdoors, the wind provides us with constant ventilation in all but the stillest of conditions. Indoors, without any wind, the air we exhale remains available for us, or someone else, to breathe back in. Indoor air can quickly become stale shared air.
Eventually stale air will leak out of most rooms through gaps around doors and windows, and clean air will leak in to replace it. But we can get much better ventilation by deliberately opening doors and windows (natural ventilation). This allows the natural movement of the outdoor air to supply clean air at a much faster rate forcing stale air out, meaning occupants are far less likely to be inhaling each other’s breath.
In a small proportion of schools and in many commercial buildings, natural ventilation is replaced with mechanical ventilation, usually built-in to the building systems. Well-managed mechanical systems are better for managing heat, comfort and energy consumption but are not necessarily superior for cleaning the air.
Improving ventilation may also have advantages of improved learning in schools and improved worker productivity (see a previous blog).
Measuring ventilation
How can you know how effective is the ventilation in any building? Firstly, using your senses can give an approximate guide. Good ventilation can be felt as a light breeze. A stale smell or “dead” sound can indicate poor ventilation. But a more reliable method is to use a monitor to measure levels of CO2 in the air. CO2 is present in every breath we exhale. When we breathe indoors the level of CO2 in the room will rise. However, if the room is well ventilated CO2 levels can’t rise too high before the stale CO2-containing air is removed. In a poorly ventilated room though the CO2 will linger for longer, building up to higher levels.
CO2 is relatively easy to monitor with moderately priced devices. This means that measurements of CO2 levels are frequently used as a proxy to estimate the stuffiness and measure if a building has adequate fresh air. High CO2 levels have been directly correlated to low productivity, as breathing in high levels can result in headaches, poor concentration, restlessness, nausea and sleepiness. If a Covid-19 infected person is in the room, a high CO2 level would indicate that the virus will also linger in the air raising the risk of infection, whereas a low CO2 level means the virus-laden air is being rapidly removed [4].
What to look for in a CO2 monitor
Wide ranges of hand-held or portable monitors are available from numerous suppliers, typically costing $100 to $500 each. They come with a varied range of features and levels of quality. A crucial consideration in selecting a CO2 monitor is whether it genuinely measures CO2. Several monitors marketed as monitoring CO2 actually do not – they measure volatile organic compounds, which are correlated with CO2 when fossil fuels are burned, but they do not respond to human breath. Most monitors come with a clear display of the current CO2 level and others additionally provide parameters such as temperature, humidity and particulate matter. Although this can be useful it is important that users can easily find the CO2 level. Another key consideration is whether the CO2 data are recorded. This can be extremely useful for reviewing the data over the full day at a convenient time or providing the data to others who can perform a more detailed analysis.
How to measure CO2
CO2 is measured in the units of parts per million (ppm). Outdoor CO2 is always equal to the background level of 412 ppm (rising at about 2.4 ppm per year as a result of global carbon emissions), or slightly higher due to nearby traffic and other combustion sources, seasonal variation in uptake from vegetation and other fluctuations due to the weather. CO2 in our breath is about 38,000 ppm. An easy way to check that a CO2 monitor is functioning is to breathe on it – values should jump up by a few hundred ppm within seconds.
Limitations of using CO2 as a proxy for ventilation
The sensitive nature of CO2 means that basing decision-making on data from a CO2 monitor needs to be considered carefully, because the location of the monitor is critical in obtaining reliable data [5]. A momentarily high value (breathing on the monitor) is not relevant for Covid-19 risk management and should be disregarded, because it may not be a true representation of the CO2 levels in the room. However, the average CO2 level over a whole day can only be assessed at the end of the day and if the data is stored and retrievable.
A system where “live” CO2 levels (some monitors have a “traffic light” green-yellow-red indicator) are used to prompt a person in the room to increase ventilation (open doors or windows, or turn on a fan) can be effective. However, these prompts are easily missed and forgotten. Conversely, such an approach can become all-consuming. In both cases they can be a source of anxiety.
Very high values (3000 ppm) should certainly be acted upon immediately. However, a system in which data are stored and reviewed over several days (ideally automatically) is probably preferable to identify rooms with persistent issues that need attention.
Ventilation in New Zealand schools
Ventilation is very important in the school environment as classrooms are typically more crowded than houses or offices. In New Zealand all new schools, and schools that have had recent upgrades are required to have CO2 monitors in classrooms as part of an ongoing Ministry of Education programme. The Ministry guideline values for CO2 first set in 2017 [6] are currently being reviewed. Many international organisations have recommended lower guideline values to ensure the extra ventilation needed to prevent transmission of COVID-19 in schools (e.g. an 800 ppm (average) recommended by the CDC), although no international consensus has yet been reached.
School case study
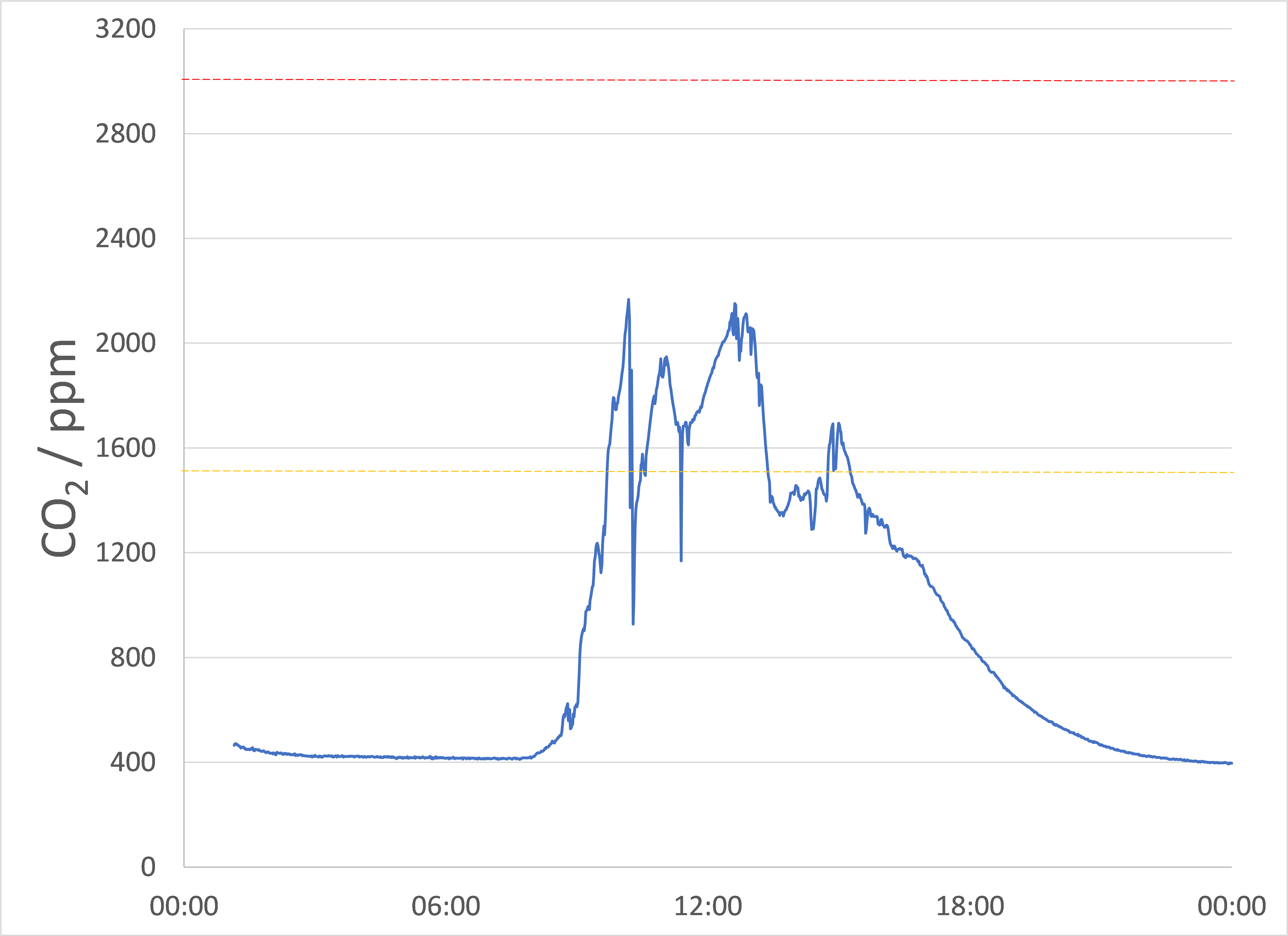
When children enter a previously empty typical classroom in the morning, CO2 will rise from the background level and often keep rising for 1-2 hours after the children have left. In fact, CO2 can often fluctuate a lot during the school day as children come and go, switch from sedentary or active, maybe open or close a window (and perhaps breathe on the monitor for fun).
An example of classroom CO2 data from a NIWA research project is shown in the Figure. On this day, this classroom met the existing Ministry of Education guideline of under 3000 ppm as a maximum value, but did not meet the school-day average guideline (under 1500 ppm at the time of this project) [6]. The highly sensitive nature of CO2 to classroom occupancy, student activity and ventilation means that CO2 levels can also vary substantially from day to day. Average daily CO2 in the classroom featured in the ranged from 886 to 1620 ppm over the course of 10 days.
Figure: CO2 levels in a typical NZ classroom (source NIWA)
The figure also shows how CO2 fell rapidly at a few times in the day, probably relating to doors being opened. However, after the school closed at around 4pm, the CO2 levels fell only slowly, not returning to background levels until midnight. This was because ventilation was reduced to a minimum when windows and doors were shut. This means children’s breath was still present in the room many hours after the children had left. Similarly, any virus particles exhaled in the classroom would also still be present many hours later. This indicates the importance of “flushing” (opening all windows and doors for 15 minutes each hour) a room with clean air before it is vacated or before it is re-occupied.
Mis-use of CO2 monitors
There are reports from overseas of wealthier parents buying CO2 monitors to pack into their children’s school bags. In principle, and given the huge numbers of classrooms in New Zealand, any means of getting more CO2 data collected could be a good thing. However, there is substantial risk of erroneous and poor quality data being collected, data being misinterpreted, cherry-picked and used in a way that is not helpful, let alone the potential to perpetuate privilege and inequity. To be valuable, such “crowd-sourced” data would still need to be collected in a way that is robust and traceable according to ethical standards that are agreed by principals, teachers and the Ministry of Education. Other models of distributing monitors are also worthy of consideration, such as monitor lending libraries and self-build kits, so long as standards are agreed to and maintained.
Conclusion
Good ventilation is one public health measure to reduce the risk of Covid-19 transmission and it may have additional advantages of improved learning in schools and improved worker productivity. If used correctly, CO2 monitors provide an indication of when to take action and can indicate which school or workplace buildings may need additional mitigation. Nevertheless, ventilation alone cannot protect people from transmitting Covid-19 and should be combined with other measures such as vaccination, mask use, staying home when unwell, and air filtration.
* Author details
Dr Ian Longley is a Principal Scientist at NIWA who leads the “Impacts of Air Pollutants” programme. He has worked in air quality research at NIWA since 2007 before which he conducted research in at the University of Manchester. Ian is a specialist in air pollution exposure science and the air quality impact of the built environment.
Dr Julie Bennett is a Senior Research Fellow at the Department of Public Health, University of Otago, Wellington. She has a wide range of public health research interests, with a particular focus on infectious diseases, indoor air quality, housing and health.
References
[1] Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. 2020; 323: 1610-1612.
[2] Mittal R, Ni R, Seo J-H. The flow physics of COVID-19. Journal of Fluid Mechanics. 2020; 894: F2.
[3] Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020; 142: 105832.
[4] Peng, Z, Jiminez, JL. Exhaled CO2 as a Covid-19 infection risk proxy for different indoor environments and activities. Environ Sci Technol. 2021; 8,5,392-397.
[5] Ackley, AU. Measuring Indoor Environmental Quality (IEQ) in a National School Property Portfolio. In Victoria University of Wellington. Open Access Victoria University of Wellington | Te Herenga Waka. Published Doctoral Thesis. 2021 https://doi.org/10.26686/wgtn.14050715.v1
[6] Ministry of Education. Designing quality learning spaces: Indoor air quality and thermal comfort. 2017.


Airborne transmission of the virus (SARS-CoV-2) causing Covid-19 has been recognised by the World Health Organization, which states that the virus can spread in “poorly ventilated and/or crowded indoor settings”. This is also the case with the US Centers for Disease Control and Prevention (CDC), which recommends: “adequate ventilation and avoidance of crowded indoor spaces”. (Your first para).
Everyone should read “The 60-Year-Old Scientific Screwup That Helped Covid Kill”
by Megan Molteni in “Wired” Magazine, May 2021
https://www.wired.com/story/the-teeny-tiny-scientific-screwup-that-helped-covid-kill/
The WHO and the global network of officials “worked to” error after error – eg “no evidence of human to human transmission”. But the costliest error, partly because it was so prolonged in spite of a tsunami of evidence that was being pointed to by a constantly growing number of experts and non-experts with sound intuitions, was the failure to recognise that Covid always was almost entirely about aerosols building up indoors. By the way, this is not just about one single linked story that I am drawing on for argument; that is merely the best one. I have been collating references on Covid aerosols and their implications for a year and a half and there is an embarrassment of riches of them. I did post the list on Medium.com and because they did not like the following argument, they cancelled me permanently.
A significant part of the death toll from Covid is a consequence of THIS error about how spread even occurs, not in fact a consequence of so-called restriction scofflaws, because the restrictions were so poorly targeted and deaths occurred anyway where they were going to (aged care homes and multifamily housing) – and worse, almost all of the collateral damage from “mitigation strategies” that were poorly targeted, the damage to economies, businesses, society, and health and mortality itself, was also a consequence of this error.
The first presentation to the WHO’s experts on aerosols was made by dozens of experts on 2 April 2020. Twenty Twenty. Advice of the kind now being offered in this blog posting, should have been “orthodoxy” by the time 2020 was halfway through. The WHO’s arrogance – not just mere confusion – on this is a matter of public record and heads should be rolling.
It is quite clear what significant impact edicts from the WHO have, because there has been a global, lockstep, fanatical, imposition of BAD advice for more than a year and a half! The WHO grudgingly amended its online advice in April 2021 but it is only now, in November, that the right strategies are being “discussed” by a few experts, and nations official mitigation strategies, especially NZ’s and Australia’s, remain stuck back in early 2020 nonsense about distancing and sanitizing and so on.
One sees the officials desperate reluctance to admit such basic things as that being outdoors in fresh air and sunshine is not only perfectly safe, it is therapeutic and should have been recommended all along. The WHO could have urgently put this nonsense into reverse pronto, especially given the disgraceful displays of police brutality in Australia and other places, and it has chosen not to do so, probably because the implications for them are too great if too many people connect the dots like I have.
There have been multiple postings on Otago Public Health Expert blog now about aerosols and ventilation, but besides the seeming possibility that NZ’s dominant officials are nowhere near as competent as the posters here, even the posters here are failing to emphasize where the number one priority is for ventilation and air treatment. That is aged care homes. One also sees a kind of desperation by the officials and the network of the media and power-hungry politicians, to admit the reality that if we could just protect the aged care homes and a few other living environments that contain vulnerable people, “the rest of us” could be allowed to just get on with life – as we always should have been allowed to.
It should not be a curious layperson like me spelling this out to the health experts – but it is obvious that the deadliness and seriousness of Covid infection correlates strongly to the “dose” of inhaled aerosols, and this is a factor of the concentration of aerosols in the indoors air, and the duration that people are present inhaling the infectious air. In aged care homes this happens to be 24/7; it is NOT just a matter of the residents being “more frail” – they are being exposed to maximum risk as well. The reason that the great majority of infections among the general public are so mild is that they were contracted in exposure durations measured in minutes or perhaps hours, rather than days. Deaths from shorter exposures invariably involve a higher concentration of aerosols, resulting from such factors as a congregation singing their lungs out in church for an hour or two.
More than a year ago, the global network of officials and politicians should have been proposing an “Apollo project” for ventilation and air treatment in aged care facilities and high-risk public environments like churches, and also in multi-family housing both public and private. The strategies actually adopted probably increased the death toll relative to a counter-factual alternative where people including rest home residents, were instructed to use fresh air, including outdoors time as well as open windows, as a mitigation strategy. An especially spectacular “own goal” concerns crowded multi-family housing where in normal circumstances, people would come and go and stay out of each others faces as much as possible – lock them down and any spread of disease that was likely to occur among those people, will occur quicker and more severely. And some people who live in these conditions are aged care home workers!
To be discussing these issues so belatedly is bad enough, but for the focus to be on schools just compounds the situation. Schoolchildren are less likely to die of Covid than rest home residents are, by a factor of some several hundred. In fact asymptomatic gaining of natural immunity is the norm to be expected in schools, and in so far as they are locations of “community spread”, that only matters to the extent that we are failing to protect or offer the right protective advice to the vulnerable who are located somewhere else entirely and can choose the circumstances under which they encounter school-aged relatives. Nor is Covid likely to rate any more significantly as a cause of death for school children, than motor accidents, suicides, falls, electrocutions, natural disasters, cancer and the normal seasonal flu.
So why this continual “missing the point” on the part of our expert institutions?